permanent restrictions after shoulder replacement
 Total Shoulder Replacement Surgery, Orthosports Orthopaedic Surgeons
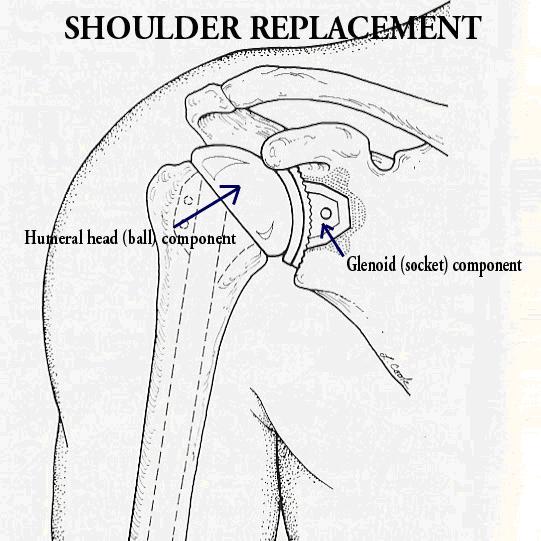
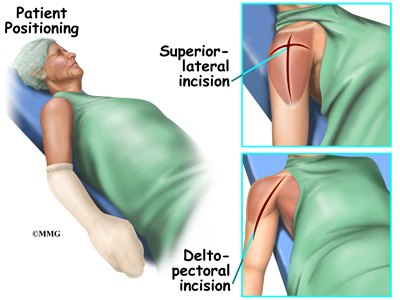
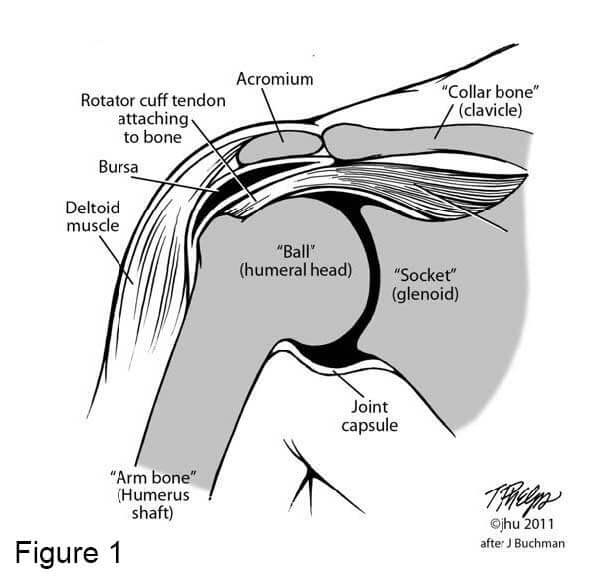
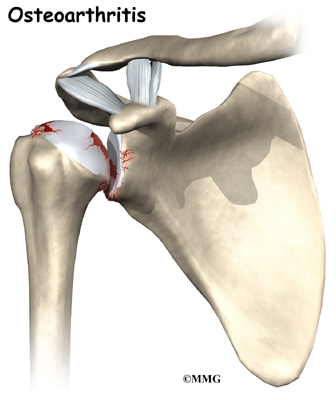
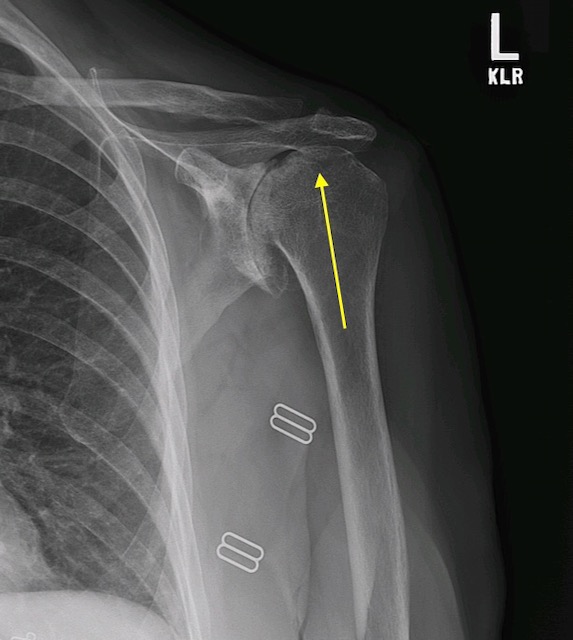
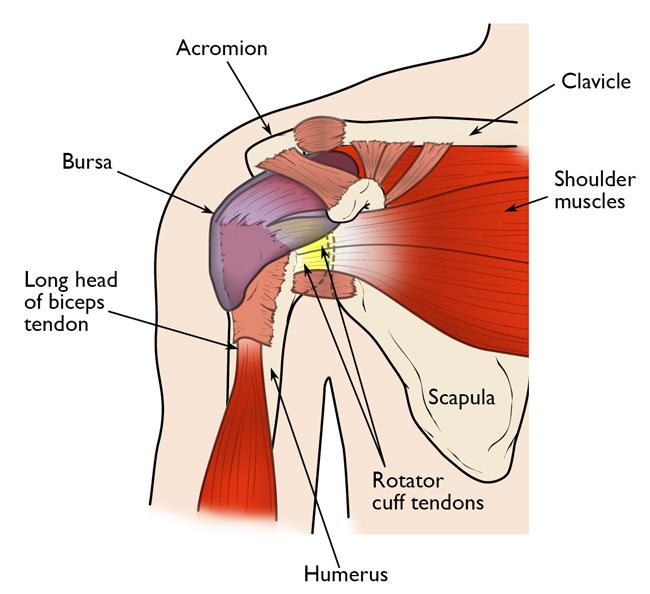
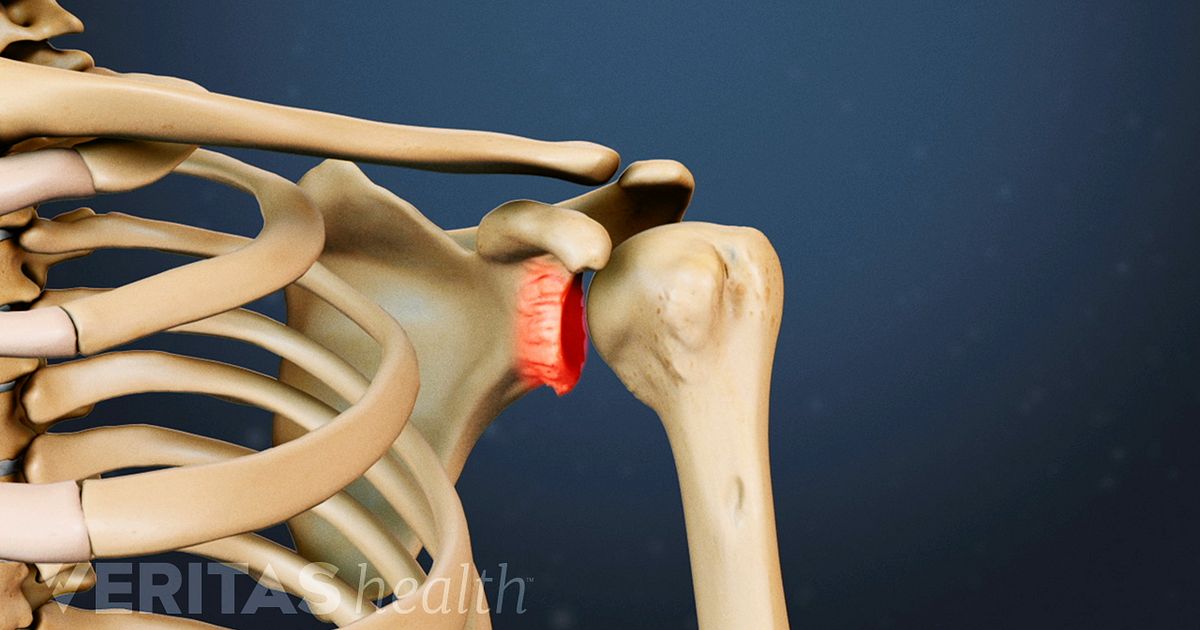
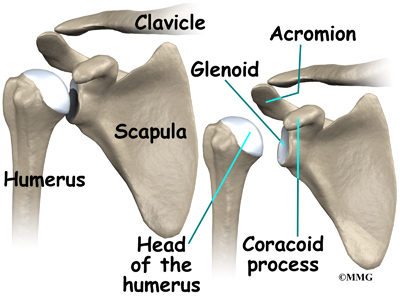
Total Shoulder Replacement Surgery, Orthosports Orthopaedic SurgeonsCall 603.742.2007 Silence-free call 800.429.5002 Silence Total Shoulder Replacement Surgery for OsteoarthritisThe shoulder arthritis is a condition in which the cartilage in the wet head and the glenoid deteriorates. The progressive use of joint surfaces can expose areas of raw bone. As this process becomes more advanced, the joint surfaces become rough, and the joint movement causes friction and abrasion. The capsule surrounding the shoulder joint can be swollen and contracted. These processes cause pain, stiffness and loss of function. The figure on the right shows the surface of a humeral head destroyed by arthritis. The cartilage has completely worn out in the central area of the ball. The X-rays of a typical arthritic shoulder show a complete loss of the joint space with bone-in-spanish joint. View on the extreme right shows how the ball is using the back of the wall of takingWhen symptoms begin to interfere with daily life activities and negatively affect the quality of life of one, it may be considered joint replacement surgery. This is the most reliable solution for shoulder arthritis that has not responded to a rest, flexibility and strengthening exercise program, and anti-inflammatory drugs. The following sections will describe in greater detail the surgical procedure, recovery period and long-term expected results after total shoulder replacement surgery. We will also discuss potential risks and complications, and long-term restrictions. Shoulder replacement surgery may improve the shoulder mechanics, but cannot do the joint as good as before the start of the arthritis. In many cases, tendons and muscles around the shoulder have weakened from prolonged disuse before operation. It can often take months of mild exercises before the shoulder achieves the maximum improvement. The effectiveness of the procedure depends on the patient's health and motivation, the shoulder condition and the surgeon's experience. The strict adherence to the rehabilitation program maximizes the possibilities of a good result of shoulder replacement surgery. Maintain general health, fitness and nutrition, as well as abstinence of smoking cigarettes, all possibilities of success. The greatest improvements are the patient's ability to sleep, to perform daily life activities and to perform non-contact recreational activities. Consideration of Surgery When normally smooth surfaces of the shoulder joint are severely damaged by arthritis or injury, the replacement surgery of the shoulder is the most effective method to restore comfort and function to the joint. There are other surgical options for the treatment of shoulder arthritis, but none have proven to be effective in terms of pain relief and patient satisfaction as a shoulder replacement. The operations of the slag or "cleanness" may be beneficial at the beginning of the course of the disease, but it has not been shown to provide lasting relief from long-term pain. The shoulder fusion operations avoid any movement in the ball and the coupling. Although this is effective in terms of pain relief, patients are limited in terms of mobility and function. Removing the joint, or resection arthroplasty, allows some movement in the joint, but does not provide strength and return to functional activities. Who should consider shoulder replacement? Shoulder replacement surgery is considered when: What happens without surgery? The natural history of arthritis is that it usually continues to progress over time. The rate of progression varies between individuals and is unpredictable. Sometimes the pain and stiffness of the shoulder arthritis will stabilize at an acceptable and manageable level for the patient. In general, this surgery is elective, and can be done when the patient decides that arthritis has become sufficiently disabled to justify treatment. In the case of osteoarthritis that delays the surgery usually does not compromise the success of the surgery in the future. Long-term considerations: As with the joint replacement procedures in other parts of the body, the components used in the replacement do not last forever. Just as the brakes of a car are degated with use, the plastic taking used in total shoulder replacement surgery also tends to be used over time. It is because younger patients are more likely to experience the wear of the shots in the course of their life, as the plastic is exposed to a longer period of use. In addition, patients who remain physically active often place greater demands on the shoulder. As more people continue to participate in sports and other demanding recreational activities in their 60s, 70s and 80s, shoulder replacements are asked to tolerate more wear and tears, often the same level of use that may have predisposed the shoulder to develop arthritis in the first place. In some cases of very active patients, the loosening of the shoulder may occur in the first years after surgery. Recognizing this potential risk, younger and more physical patients may be better with a partial joint replacement that does not surpass the arthritic socket. Effectiveness: Shoulder replacement surgery for osteoarthritis has shown an effective means of restoring the lost comfort and function to the shoulder. However, it must be recognized that certain limitations on mobility and force may persist after surgery. This is because the muscles, tendons and ligaments around the shoulder joint can be contracted or atrophied from the arthritis process. Some of these changes may not be reversible with surgery. There are several factors that influence the effectiveness of the surgery and should be considered in the light of the decision to replace the shoulder: In general, 90% of patients report excellent results after the replacement surgery of the shoulder. Emergency:Shop replacement surgery for osteoarthritis is an elective procedure that can be programmed when circumstances are optimal for the patient. It's not an urgent procedure. The patient has a lot of time to be informed about the surgery and recovery process. The factors that the patient should consider when choosing the optimal time include the following: Preparation for SurgeryPreparation The success of the surgery depends on an association between the patient and the experienced shoulder surgeon. Patients should optimize their health so they are in the best possible condition for this procedure. Smoking should be stopped one month before surgery and not resumed for at least three months later to maximize the healing potential of the body. Any heart, lung, kidney, bladder, tooth or gum problem should be handled before surgery. Any infection can be a reason to delay the operation. The shoulder surgeon should be aware of all health problems, including allergies and prescription and prescription medications being taken. Some of these may need to be modified or stopped. For example, aspirin and anti-inflammatory drugs may affect the way blood clots. If patients take medications for bleeding such as Coumadin, they should consult with their primary care doctor for the safety of stopping their use 5-7 days before the procedure. These medicines can usually be resumed the day after surgery. The incision for a shoulder replacement extends across the front of the shoulder from the outer end of the neck bone to the middle end of the upper arm. This area should be kept clean and free from cuts or scratches leading to surgery. The necessary assistance plans should be made before the surgery. For people living alone or without help available, arrangements should be made for home help during the initial recovery period well in advance. Many patients will benefit from a stay in a rehabilitation center for a period after surgery until they recover enough to manage with daily activities. Surgical equipment replacement surgeryShoulder is a technically demanding procedure that should be performed by an experienced surgeon in a medical center used to perform shoulder joint replacements at least several times a month. While most general orthopaedic surgeons perform 1-2 hip or knee replacements per month, the average surgeon can only perform 1 shoulder replacement per year. Dr. Parsons is widely trained in these procedures, having advanced training of specialty in the field of shoulder surgery in one of the most occupied shoulder replacement centers in the country. This included training in managing complex and failed shoulder replacements. Ours Surgical equipment includes dedicated staff experienced in performing these procedures and carefully select our implants based on the best products available for individual cases. About surgeryTechnical details Replacement of the shoulder for osteoarthritis is a highly technical procedure; each step plays a critical role in the result. After the anesthesia has been administered and the shoulder has been prepared, an incision is made on the front of the shoulder from the center of the collarbone to the center of the arm bone. This incision allows access to the joint without damaging the major deltoid or pectoralis muscles that are responsible for a significant part of the shoulder power. Muscles and other tissues close to the shoulder are mobilized by removing any scar tissue that may restrict your movement. The subscapular muscle tendon is cut to gain access to the joint and is released circumferentially to restore its length and mobility. The artritic humeral head is dried together with the bone spades surrounding it. This cut should be carefully planned and aimed at recreating the anatomy of one with reconstruction. The humeral implant is chosen by the rehearsal of different sizes and the selection of which best fits the anatomy of patients and best restores the muscle balance in the joint without making the joint too tight or too loose. The arthritis glynoid is then exposed to the elimination of all bone spades from its periphery. The proper exposure is a challenging process, and the surgeon must be familiar with the location of important nerves and blood vessels. A special re-emer is used to refine the glenoid surface in preparation for the prosthesis. This remembrance process corrects the form and orientation of the socket, both affected by shoulder arthritis. Several small holes are pierced into the socket and filled with bone cement to accept the wigs of the glenoiding prosthesis. The prosthesis is inserted and kept in place until the dry cement. A test head is placed in the humeral prosthesis to determine the right size and muscle balance. Then the final humeral components are inserted and the joint is relocated. The subscapular tendon is carefully repaired back to the bone and the closure of the muscle layers and the skin completes the procedure. A drainage is placed that is removed in the second morning after surgery. This prevents blood from collecting on the wound. The figure on the right shows a well-placed prosthesis that restores the anatomical relationship between the ball and the socket and recreates a smooth and balanced joint. Anesthetic Shoulder replacement surgery may be performed under general anesthesia or under a brachial plexo nerve block. A brachial plexo block can provide anesthesia for several hours after surgery. The patient may wish to discuss his preferences with the anesthesiologist before surgery. Duration of surgery The procedure usually lasts about two hours, however, preoperative preparation and postoperative recovery can add several hours to this time. Patients usually spend two hours in the recovery room and two to four days in the hospital after surgery. Risk and Potential Complications Complications related to shoulder replacement surgery can be divided into those that occur during surgery, those that occur shortly after surgery and those that occur in a time away from surgery Complications during the procedure include: Complications that occur shortly after surgery include: Complications that occur remotely from surgery: Recovering from surgeryDolor and pain managementRecovery of comfort and function after replacement year. The proper control of pain is an important part of postoperative management because it facilitates rehabilitation and allows the recovery of movement. Immediately after surgery, strong medicines (such as morphine) are often given by injection. Within a day or so, medications for oral pain (such as Percocet or Vicodin) are generally sufficient. These oral narcotic drugs are usually only necessary for a few weeks and patients are encouraged to get rid of them to regular Tylenol when comfortable enough. Pain medications can be very powerful and effective. Its proper use lies in balancing its pain relief effect and its other less desirable effects, such as sedation. Pain medications can cause drowsiness, slow breathing, difficulties in emptying the bladder and intestine, nausea, vomiting and allergic reactions. Patients who have taken substantial narcotic drugs in the recent past may find that the usual doses of painkillers are less effective. For some patients, it is difficult to balance the benefit and side effects of pain medication. Patients should notify their surgeon if they have had previous difficulties with pain or pain control medications. We generally discourage the use of anti-inflammatory drugs (such as Ibuprofen, Advil, Motrin, Naprosyn) unless patients require their use for other conditions. These medications can stop the healing of the subscapular tendon. Ice is used to decrease pain and inflammation during initial recovery and for several weeks during rehabilitation. Hospital Stay and Hospital DischargePatients usually stay in the hospital for 2-4 days after replacement surgery. The criteria for discharge, whether at home or in a rehabilitation hospital include: 1. a clean and dry incision without signs of infection 2. normal function of the intestine and bladder 3. proper pain relief with oral pain medications 4. Ability to perform and properly fulfill the home movement exercise program 5. Suitable support to ensure that patients are safe if they return to the home environmentBecause surgical repair should be protected by limited arm use during the first 6-8 weeks after surgery, it should be prepared to manage daily activities with a very limited use of the arm involved. The patient is usually asked not to lift anything heavier than a cup of coffee during this time. Patients usually require some self-care assistance, daily life activities, shopping and driving for about six weeks after surgery. The management of these limitations requires early planning to carry out daily life activities during the recovery period. If sufficient assistance is not available to assist these basic activities, a rehabilitation stay is recommended for the overall safety of the patient, as well as for the safety of the surgical reconstruction. RehabilitationRecovery and Rehabilitation in the Hospital Early movement after shoulder replacement surgery helps to achieve the best possible shoulder function. The arid shoulders are stiff. The early movement is facilitated by the complete surgical release of tight tissues so that after surgery the patient only has to maintain the range of movement reached in the operation. However, after surgery, the scar tissue will tend to recite and limit the movement unless the movement starts immediately. Early motion also stimulates recovery of muscle function. During hospitalization, the patient learns a simple rehabilitation program that will be used to maintain the range of movement after discharge. This program consists of self-assisted front lifting and external rotation, elbow bending and the extension and strengthening of the grip. Whether on the day of surgery, or the day after surgery, the physical therapist will work with the patient to ensure the appropriate technique and understanding of the program. Walking and arm use for soft activities are encouraged shortly after surgery. Imbulatory Physical TherapyRecovering mobility, strength and function is a graduated process that follows the healing of the tissue. We have developed comprehensive therapy protocols designed to prevent recurring stiffness and re-educate muscles on the shoulder belt to operate smoothly and in a coordinated manner. These protocols are designed in such a way that the therapist will educate patients about home exercises throughout the recovery process. The exercises that a patient does for himself between therapy sessions are equally important as the sessions themselves, and the patient's adherence to this program is essential to prevent early stiffness. A properly performed domestic exercise program ensures that exercises are performed frequently, effectively and comfortably. The early recovery period focuses on maintaining the range of movement reached by the release of scar tissue during surgery. Strengthening exercises are not performed during the first 6 weeks to avoid stress in tendon repair. A sling is used between exercise sessions during the first month and can then be suspended. Patients can use the hand to hold objects like a cup of coffee or newspaper, but nothing more than 1-2 pounds. For 6 weeks, you can resume the soft active use of the arm for daily activities, but it is not allowed to lift, push or pull heavy. Therapy focuses on a program of continuous flexibility with the aim of a progressive return to every range of motion. Muscle re-education begins with light resistance exercises for rotating cuff and muscles that stabilize the shoulder blade. For 3 months, patients may resume full use of the limb provided they have reached a functional active range of motion. Progressive strengthening exercises with greater resistance and resistance exercises such as swimming, rowing and upper ergometer of the body are encouraged. In addition, we strongly encourage an aerobic conditioning program for the lower extremities to promote general health and physical fitness. By following this exercise program, patients are almost always satisfied with the increases in the range of movement, comfort and function they achieve during the recovery period. If the exercises are uncomfortable, difficult or painful, the patient should contact the therapist or surgeon promptly. Maintenance rehabilitation Once movement and force objectives are reached, the exercise program can be reduced to a minimum level. However, soft stretching is recommended continuously. In addition, a maintenance program to maintain the muscles of the strong and healthy rotating cuff will ensure the proper function of the artificial joint and can help prolong your benefit. Back to Functional and Recreational Activities With the consent of your surgeon, patients can often return to activities such as swimming, golf and tennis at 4-6 months after your surgery. It is essential that patients reach a sufficient range of movement and force beforehand to prevent muscle fatigue and undue stress in artificial components. Limitations of long-term patients Activities involving a significant impact load on the shoulder joint (such as cutting wood, contact sports, heavy weight lift hammer, etc.) may jeopardize the performance of joint replacement. These types of activities increase the risk of loosening, wear and fracture of artificial socket and may also risk sguince or tearing of the rotating cuff. Therefore, patients should be careful in this type of activity to minimize the risk of shoulder damage. How long will the shoulder replacement last? A properly performed shoulder replacement usually lasts between 10-20 years. Factors that determine the longevity of the prosthesis include age, handsholding, physical demands, compliance with limitations among others. The duration of the comfort and function offered by a shoulder replacement cannot be predicted in advance in any given case. Revision surgery for a failed shoulder replacement often involves removing a used or broken socket. These procedures are very technically demanding but generally successful in restoring the shoulder function. In general, however, the results of the review of the replacement of shoulders are not as good as for the replacement of primary shoulders. Download This resource has been provided by Seacoast Orthopedics and Sports Medicine as general information only. This information cannot be applied to a specific patient. Places and Contact Follow us on TwitterAs we on FacebookThere are no recent Facebook posts to show

Can I avoid shoulder replacement surgery? The evidence for shoulder replacement alternatives – Caring Medical Florida
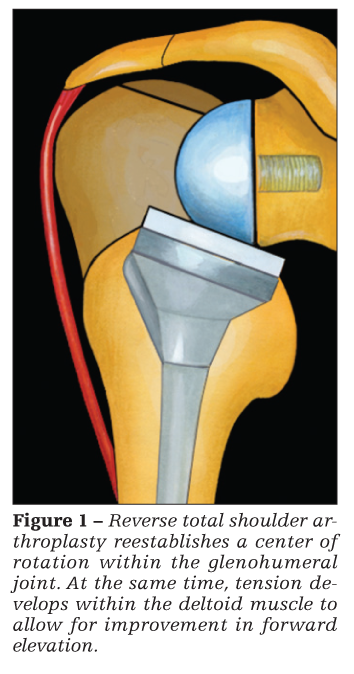
Reverse Shoulder Arthroplasty | eOrthopod.com

Reverse Shoulder Replacement | UW Orthopaedics and Sports Medicine, Seattle
Failed Rotator Cuff Repairs | Johns Hopkins Shoulder and Elbow Surgery
Patient guide to shoulder replacement.
The Reverse Shoulder Replacement Book
For Total Shoulder Replacement
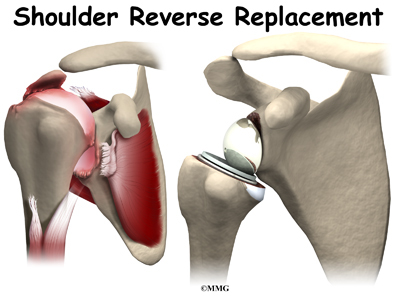
Reverse Shoulder Arthroplasty | eOrthopod.com
The Shoulder Replacement Book

Range of Motion After a Total Shoulder Replacement
Reverse Shoulder Arthroplasty | eOrthopod.com
Physical Therapy Guide to Shoulder Replacement (Arthroplasty) - ChoosePT.com
Anatomic Shoulder Arthroplasty and Reverse Ball Socket Arthroplasty

Shoulder Replacement: Recovery, What to Expect, Risks, and More
Limitations After Reverse Shoulder Replacement? | Dr. Chris Jones
Anatomic Shoulder Arthroplasty and Reverse Ball Socket Arthroplasty

What to Expect After Your Shoulder Arthroscopy and Labral Repair
The Shoulder Replacement Book

How long does a shoulder replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 10 years of follow-up - The Lancet Rheumatology

Range of Motion After a Total Shoulder Replacement

Reverse Shoulder Arthroplasty | eOrthopod.com

What to Expect After Your Shoulder Replacement | Dr. Gombera

Reverse Shoulder Replacement | UW Orthopaedics and Sports Medicine, Seattle
Rotator Cuff Tears - OrthoInfo - AAOS
The Reverse Shoulder Replacement Book

Shoulder Replacement Surgery Failure & Lawsuit - Schwaner Injury Law
The Ins and Outs of a Reverse Shoulder Replacement

Rotator Cuff Tears: Surgical Treatment Options - OrthoInfo - AAOS

Why Elbow Replacements Are More Common Than Ever (Hint: It's Not Just for Arthritis Anymore) – Health Essentials from Cleveland Clinic
Current Issues in Reverse Total Shoulder Arthroplasty
Shoulder Replacement Surgery

What to Expect After Your Shoulder Replacement | Dr. Gombera

Ream And Run Shoulder Resurfacing Replacement
Patient guide to shoulder replacement.
Anatomic Shoulder Arthroplasty and Reverse Ball Socket Arthroplasty

Basics of Failed Shoulder Surgery | UW Orthopaedics and Sports Medicine, Seattle

Frozen Shoulder (Adhesive Capsulitis) Treatments
Reverse Shoulder Arthroplasty | eOrthopod.com

When Can I Start Working Out After Shoulder Surgery?

Managing Massive Irreparable Rotator Cuff Tears - Cancer Therapy Advisor
Posting Komentar untuk "permanent restrictions after shoulder replacement"